Brachial Plexus Palsy: Erbs Palsy Treatment
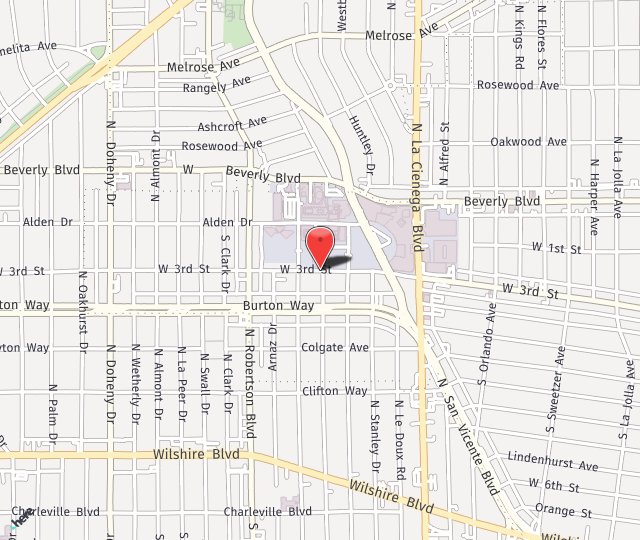
in Los Angeles CA
What is Brachial Plexus Palsy?
Have you felt a weakness in your arm? Maybe you have noticed a lack of arm movement in your baby? Whether you or a loved one is experiencing this condition, Dr. Seruya of the Los Angeles Nerve Institute is here to help.
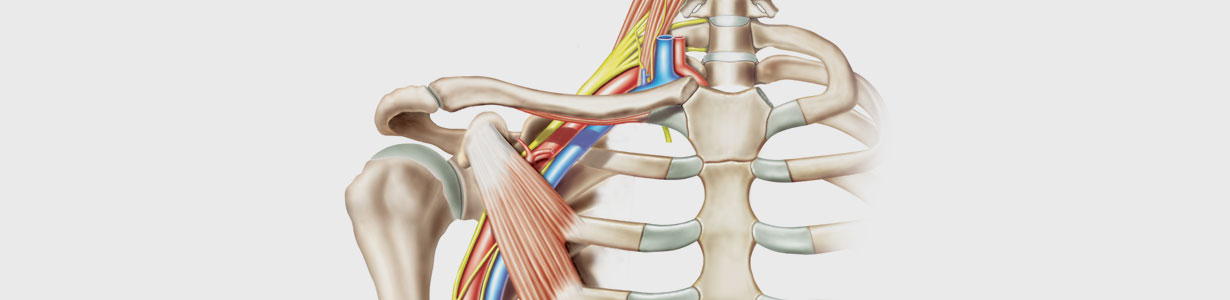
The brachial plexus is a network of nerves that extend from the neck into the arm. Five major nerves (given the symbols C5, C6, C7, C8, & T1) exit from the spinal cord in the neck to provide movement and feeling to the arm and hand. In Brachial Plexus Palsy, any one of these five main nerves may be injured. When the upper nerves (C5, C6, +/-C7) are injured, the patient has what is called Erb’s Palsy. When nearly all nerves have been injured, the patient has what is called Total or Complete Brachial Plexus Palsy.
Los Angeles Nerve Institue offers treatment for Brachial Plexus Injuries and Erb’s Palsy in Los Angeles.
Can My Primary Care Doctor Evaluate Me For Erbs Palsy?
- Electromyography (EMG) — A needle is inserted into various muscles. The electrical activity of the muscles is evaluated when they contract and when at rest.
- Nerve conduction studies — These tests usually accompany EMGs. They measure the speed of conduction in your nerve when a small current passes through the nerve. This shows how well the nerve is functioning.
- Magnetic resonance imaging — MRIs use powerful magnetic and radio waves to produce detailed views of your body in multiple planes. MRIs can show the extent of the damage caused by a brachial plexus injury.
- Computerized tomography myelography — CT scans use a series of x-rays to create cross-sectional images of your body. CT myelography adds a contrast material, injected during a spinal tap, to produce a detailed picture of your spinal cord and nerve roots during a CT scan.
If you’re exhibiting signs of nerve damage, it’s likely to be necessary to contact a nerve specialist such as Dr. Seruya.
Erbs Palsy Symptoms
When nerves of the brachial plexus are injured, the electrical signals in them stop traveling to or from the brain. Muscles of the arm and hand no longer receive electrical signals from the brain to make them work. These muscles turn off and the patient may become weak or paralyzed in the shoulder, elbow, wrist, and/or hand. Not only can patients lose strength, but they can also lose feeling in the skin of the arm and hand. Patients may refer to this as numbness.
Causes Of Brachial Plexus Palsy
Brachial Plexus Palsy may occur during birth, following trauma, or from radiation, tumor, or a virus. Depending on the situation, the nerve can be injured by stretch, rupture, avulsion, or direct damage. In stretch-type injuries, the inner part of the nerve remains together but is its outer cover and blood supply are pulled apart. In rupture-type injuries, the nerve completely snaps and leaves two free ends that are no longer talking to each other. In avulsion-type injuries, the nerve is directly pulled off its electrical source in the spinal cord. Indirect damage, the nerve is injured by radiation or tumor or by the virus turning it off.
Diagnosing Erbs Palsy
Erb’s Palsy can generally be diagnosed by the history and by physical exam looking for signs of weakness or numbness along the shoulder, elbow, wrist, and/or hand. In situations where the diagnosis is unclear, a nerve conduction and muscle study can be ordered to obtain more information on the health of the individual nerves and their muscles. An MRI can also provide a picture as to the type of brachial plexus injury.
Preparing For Your Erbs Palsy Surgery
You’ll prepare for these procedures as you do with any surgery. A few days prior to your surgery with Dr. Seruya you’ll stop taking any blood thinners, anti-inflammatory medications, and most supplements. If you smoke, you’ll need to stop for one month prior to your surgery and one month afterward, as smoking inhibits wound healing. We’ll discuss other specifics leading up to your surgery.
Options
Treatment for Erb’s Palsy in Los Angeles begins and ends with occupational therapy. An occupational therapist scores the strength of each muscle group. The amount of motion at each joint is measured to identify areas that are tight. Patients then begin stretching exercises to keep the joints loose and work on strengthening. At each visit, the muscle scores and joint motion will be compared. Patients who are not making gains over several months are advised to undergo surgical treatment. Surgery is recommended when it is believed that the chances of achieving further recovery are better with nerve reconstruction than waiting for the nerve to heal on its own.
Patients should understand that there isn’t an unlimited time that you can wait to fix the nerves. By 12-18 months, the nerve permanently loses its connection to the muscle. After then, even if the injured nerve is reconstructed, it won’t be able to tell the muscle to contract. Taking that into account, and the fact that a repaired nerve heals at 1 mm a day, the timing of surgery directly depends on the location of paralysis. If the hand is paralyzed, surgery is offered by 3 to 4 months to give the nerve enough time to reach its muscles before that special connection is irreversibly lost. If the elbow is paralyzed, surgery is offered by 4 to 6 months.
For shoulder paralysis, surgery may be offered by 6 to 9 months. Surgical treatment focuses on healing the injured nerve(s). This may include one or more of the following: 1) removing scar tissue from around the nerve to allow the electrical signals to travel more easily across the nerve (nerve decompression/neurolysis); 2) cutting out the scar tissue that is filling the nerve gap and bridging it with a sensory nerve (nerve graft); 3) selecting a motor nerve from a healthy but less important muscle group and transferring it to an injured nerve that is more important to shoulder elbow, or hand function (nerve transfer).
What Is The Success Rate For Brachial Plexus Palsy Surgery?
If surgery is required, it needs to occur within six months of the patient’s injury. Dr. Seruya has had good success with these procedures when they occur in that timeframe. The longer you go without a nerve stimulating a particular muscle, success rates drop, as there is less chance the muscle will ever function normally again.
Real Brachial Plexus Injury Patient Experiences
“Dr. Seruya changed our lives! He operated on our daughter Dylan who had shoulder dystocia and a brachial plexus injury. He did a nerve transplant surgery on her at 5 months old. We are forever grateful for him.” – M.S
“If I could give Dr. Seruya a 500 star review, it still wouldn’t be enough. My daughter suffered a brachial plexus injury at birth, due to getting stuck in the birth canal…She is going to live her life without limitations and there is no doubt in my mind that I have Dr. Seruya to thank for that. In my opinion, there is no better care for nerve treatment out there. Don’t wait to call him. He changed our life.” – M.M
Recovery From Brachial Plexus Palsy Surgery
Brachial plexus surgery is performed under general anesthesia and can last several hours. After surgery, patients are typically wrapped in a shoulder and elbow sling to protect the nerve reconstruction against the motion. For most nerve transfer procedures, patients may only need an overnight hospital stay and are discharged home the following morning. If rib (intercostal) nerves are used as nerve transfers, patients may be admitted overnight in the Intensive Care Unit as a precaution to monitor their breathing and then stay for 3-4 days before being discharged to home.
During the hospital stay, pain specialists place the patient on medications that specifically treat nerve pain. Three to four weeks after surgery, patients may take off their elbow and shoulder sling. At this point, full stretching is permitted except in patients with intercostal nerve transfers. Patients with rib (intercostal) nerve transfers must wait a total of 8 weeks before stretching the shoulder to avoid pulling the nerve connections apart. Patients will be followed closely by occupational therapists, who will use electrical stimulation to gently help the nerves turn back on. Each patient’s recovery is different.
Risks Of Erb’s Palsy Surgery
Risks associated with surgery to repair a brachial plexus injury include failure to improve the situation, tingling or diminished strength in areas of the hand or forearm, and post-surgical stiffness. Tingling and strength issues usually are only temporary. The risks are low in these surgeries considering the risks involved in not having the damaged nerves repaired. If the nerves are not repaired the patient will be at risk for losing complete function and use of the muscles served by the nerve, such as those in the hand or arm.
What Happens If Erb’s Palsy Is Left Untreated?
You can’t leave nerve damage untreated. Nerves that aren’t healing on their own have a limited time to be repaired with surgery or they will lose their connection to the muscles they serve. Once that happens, even if the injured nerve is reconstructed it won’t be able to control the muscle.
Nerve damage with brachial plexus palsy is not something to “tough out.” If you do, you’re likely to have permanent loss of function in the area impacted.
What Can I Expect During Occupational Therapy For Brachial Plexus Palsy?
With newborns whose injury was due to a difficult delivery, occupational therapy focuses on keeping nearby muscles and joints strong and loose as the nerves heal. The parents are instructed on how to protect the newborn’s arm and shoulder during feedings, clothing changes, and other daily activities. The parents are also shown how to perform gentle exercises at home on the baby’s shoulder, elbow, and wrist.
For adults, occupational therapy is the beginning and end of treatments of all Erb’s Palsy treatments, whether surgical or non-surgical. Your occupational therapist will help you perform the normal activities or tasks in life that have been impacted by your nerve injury.
During your first appointment, your OT will assess your needs. They may come to your home or workplace to see what you do and what changes you need to make. Next, they’ll develop a plan for therapy and set goals for you to either improve movements or to find new ways of performing them.
If surgery is involved, occupational therapy has already been tried but patients haven’t been improving. Surgery is then recommended. OT will be combined with physical therapy after surgery to regain strength and, if needed, to retrain muscles that have been disabled.
Schedule a Consultation
For additional information on Brachial Plexus Palsy or Erb’s Palsy treatment in Los Angeles, CA, call our office at (310) 423-2129 to schedule a consultation today!


 “Dr. Seruya changed our lives! He operated on our daughter Dylan who had shoulder dystocia and a brachial plexus injury. He did a nerve transplant surgery on her at 5 months old. We are forever grateful for him.” – M.S
“Dr. Seruya changed our lives! He operated on our daughter Dylan who had shoulder dystocia and a brachial plexus injury. He did a nerve transplant surgery on her at 5 months old. We are forever grateful for him.” – M.S