Facial Paralysis | Bell’s Palsy | Los Angeles, CA
What is Facial Paralysis? (Bell’s Palsy)
Facial paralysis may occur from birth, following trauma, or from radiation, tumor, or a virus. The facial nerve (Cranial Nerve VII) powers the small muscles of the face that cause the eyelids to blink and mouth to smile.
Facial Paralysis is a condition where the facial nerve is partially or completely injured. Sometimes, facial paralysis is also referred to as Bell’s Palsy. Weakness can involve one (unilateral) or both (bilateral) sides of the face.
What are the symptoms of Bell’s Palsy?
When the facial nerve is injured, the electrical signals in it stop traveling from the brain to the facial muscles. Muscles around the eye and mouth no longer receive these electrical signals and turn off. Simple tasks such as blinking or making a smile become hard, if not impossible. If the eyes cannot close, they will dry out and develop redness. Over time, patients can experience vision loss if the clear layer in front of the eye (cornea) dries out and is damaged. Other common symptoms include drooling from the weak corner of the mouth.
What causes Facial Paralysis?
Facial paralysis may be present at birth (congenital, Moebius syndrome, hemifacial microsomia), following trauma, or result from radiation, tumor, or viral illness. Other risk factors include diabetes and recent upper respiratory tract illness. Depending on the situation, the nerve can be injured by stretch, rupture, avulsion, or direct damage. In stretch-type injuries, the inner part of the nerve remains together but is its outer cover and blood supply are pulled apart.
In rupture-type injuries, the nerve completely snaps and leaves two free ends that are no longer talking to each other. In avulsion-type injuries, the nerve is directly pulled off its electrical source in the brainstem. In direct damage, the nerve is injured by radiation or tumor or by the virus turning it off in the brainstem.
See What Patients Are Saying About Us
“Compared to other doctors who would be intentionally vague and suspicious in their responses to my questions, he was eager to show me his work (one of his assistants took photos and videos during the procedures). He is an excellent physician and an honorable person, and I would recommend him to anyone experiencing nerve damage that other doctors are unable to treat.” -Richard D.
How is Bell’s Palsy diagnosed?
Bell’s Palsy can generally be diagnosed by the history and physical exam, looking for signs of weakness around the eye and mouth. Nerve conduction and muscle studies can offer more information on the health of the individual nerves and their muscles. A CT of the base of the skull and/or MRI scan can also provide a picture as to whether the facial nerve is injured due to rupture, avulsion, or by direct damage from a virus or tumor.
What are the treatments for Bell’s Palsy?
Treatment of Bell’s Palsy begins and ends with occupational therapy. An occupational therapist grades the facial movement and works with the patient on smile strengthening exercises.
Surgery is recommended when it is believed that the chances of achieving further recovery are better with nerve reconstruction than waiting for the nerve to heal on its own. Patients should understand that there isn’t an unlimited time that you can wait to fix the nerves. If within 12 months from the time of paralysis, surgical options focus on treating the injured nerve. This may include one or more of the following:
Types of Surgical Procedures for Bell’s Palsy
1. Nerve Decompression / Neurolysis
Removing scar tissue from around the nerve to allow the electrical signals to travel more easily. Read more about nerve decompression/neurolysis »
2. Nerve Graft
Cutting out scar tissue that is filling the nerve gap and bridging it with a sensory nerve. Read more about the nerve graft procedure »
3. Nerve Transfer
Selecting a motor nerve from a healthy but less important muscle group and transferring it to the injured facial nerve. Read more about the nerve transfer procedure »
Before and After Photos
Patients in this situation may benefit from transplanting a healthy muscle to the face to replace the paralyzed smile muscle (free functional muscle transfer). How to power this new muscle depends on whether the patient has paralysis on one or both sides of the face. When only one side is paralyzed, patients first undergo a procedure that borrows an expendable part of the facial smile nerve on the strong side of the face and bridges it to the injured side with a nerve graft (cross-face nerve graft).

What happens after surgery for Facial Paralysis?
Facial paralysis surgery is performed under general anesthesia and can last several hours depending on the extent of injury. For nerve procedures, patients may only need an overnight hospital stay and are discharged to home the following morning. For free functional muscle transfer, patients are monitored in the Intensive Care Unit for 3 days followed by 2 days on the hospital floor to check on the health of the newly transplanted muscle. Patients will be followed closely by occupational therapists, who will use electrical stimulation to gently help the nerves turn back on. Each patient’s recovery is different in terms of how many months it takes for the facial muscles to turn back on.
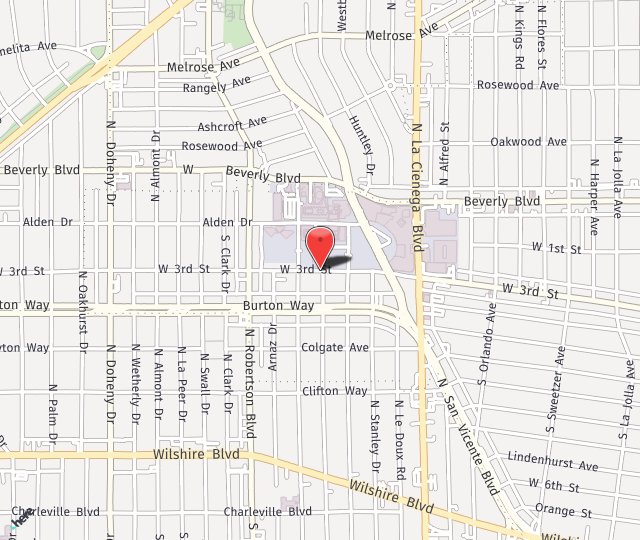
Schedule a Consultation with Dr. Seruya Today
If you are interested in learning more about our Facial Paralysis procedure options, call us today at (310) 423-2129 or fill out the contact form below. Our practice is proud to serve Los Angeles and the surrounding areas of California.

 “Compared to other doctors who would be intentionally vague and suspicious in their responses to my questions, he was eager to show me his work (one of his assistants took photos and videos during the procedures). He is an excellent physician and an honorable person, and I would recommend him to anyone experiencing nerve damage that other doctors are unable to treat.” -Richard D.
“Compared to other doctors who would be intentionally vague and suspicious in their responses to my questions, he was eager to show me his work (one of his assistants took photos and videos during the procedures). He is an excellent physician and an honorable person, and I would recommend him to anyone experiencing nerve damage that other doctors are unable to treat.” -Richard D.