Phrenic Nerve Paralysis Treatment
in Los Angeles, CA
What is Phrenic Nerve Paralysis?
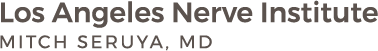
The phrenic nerve controls the diaphragm, which is the major muscle for breathing. Three major nerves (given the symbols C3, C4, C5) exit from the spinal cord in the neck and combine to form the phrenic nerve. Right and left phrenic nerves to travel between the lung and heart to power each side of the diaphragm. When breathing in, the diaphragm drops to allow the lungs to bring air in. On breathing out, the diaphragm rises to push air out. Phrenic Nerve Paralysis can involve injury of the right, left, or both phrenic nerves.
Symptoms of a Paralyzed Diaphragm

What causes Phrenic Nerve Paralysis?
Phrenic Nerve Paralysis may occur during birth, following trauma, or from radiation, tumor, or a virus. Depending on the situation, the nerve can be injured by stretch, rupture, avulsion, or direct damage. In stretch-type injuries, the inner part of the nerve remains together but is its outer cover and blood supply are pulled apart. In rupture-type injuries, the nerve completely snaps and leaves two free ends that are no longer talking to each other. In avulsion-type injuries the nerve is directly pulled off its electrical source in the spinal cord. Indirect damage, the nerve is injured by radiation or tumor or by the virus turning it off.
How is Phrenic Nerve Paralysis diagnosed?
Phrenic Nerve Paralysis can generally be diagnosed by history and by physical exam looking for signs of difficulty breathing. In situations where the diagnosis is unclear, a nerve conduction and muscle study can be ordered to obtain more information on the health of the right and left phrenic nerves and the diaphragm muscle. A standard X-ray can provide a snapshot of the diaphragm and its location. Chest fluoroscopy is an even more detailed X-ray and can show the right and left side of the diaphragm in motion as the patient breathes in and out.
Paralyzed Diaphragm Treatment in Los Angeles

Surgery is recommended when it is believed that the chances of achieving further recovery are better with nerve reconstruction than waiting for the nerve to heal on its own. Patients should understand that there isn’t an unlimited time that you can wait to fix the nerves. By 12-18 months, the nerve permanently loses its connection to the muscle. After then, even if the injured nerve is reconstructed, it won’t be able to tell the muscle to contract. Taking that into account, and the fact that a repaired nerve heals at 1 mm a day, surgery is offered by 6 to 9 months.
Surgical treatment focuses on healing the injured nerve(s). This may include one or more of the following: 1) removing scar tissue from around the nerve to allow the electrical signals to travel more easily across the nerve (nerve decompression/neurolysis); 2) cutting out the scar tissue that is filling the nerve gap and bridging it with a sensory nerve (nerve graft); 3) selecting a motor nerve from a healthy but less important muscle group (spinal accessory nerve or intercostal nerves) and transferring it to the injured phrenic nerve (nerve transfer).
What happens after surgery for Phrenic Nerve Paralysis?

Who is at risk for developing phrenic nerve paralysis?
Phrenic nerve paralysis is a rare condition, but there are certain situations or health conditions that elevate a person’s risk, including:
- Surgical trauma during a heart or neck procedure
- Injury during interscalene nerve blocks
- Injury during chiropractic manipulation of the neck
- Birth trauma that injures the phrenic nerve in newborns and infants
- Neurological diseases, such as amyotrophic lateral sclerosis (ALS), multiple sclerosis, muscular dystrophy, Guillain-Barre syndrome
- Radiation
- Cancer in the lung or lymph nodes that compresses the phrenic nerve
- Spinal cord disorders and quadriplegia
- Chest surgery where the phrenic nerve is cut or removed to remove a tumor
- Chronic pneumonia, bronchitis, or cardiac arrhythmias
- Neuropathic disease, including thyroid disease and autoimmune disease
Is phrenic nerve paralysis painful?
This condition is not painful in the acute sense of the term. It causes problems with breathing, which is thoroughly uncomfortable on its own. These problems lead to fatigue, insomnia, headaches, blue lips and fingers, and overall difficulty breathing.
What happens if phrenic nerve paralysis is left untreated?
Unless the phrenic nerve is injured on both sides, making the patient unable to breathe on his or her own, this is often an elective treatment situation. In some cases, the damaged nerve may heal on its own, but patients need to understand this isn’t an unlimited window. If nerve damage is left for over a year, there is a good chance the nerve will permanently lose its connection to the diaphragm.
Otherwise, the first step is physical therapy to strengthen the diaphragm, rib, and neck muscles. There’s no reason to not opt for this treatment as a starting point.
Are there risks involved with phrenic nerve surgery?
Phrenic nerve paralysis leads to a poor quality of life, as the person is plagued by chronic fatigue and shortness of breath. Activities the person formerly enjoyed are basically out of the question due to inherent difficulty with simple breathing. With any surgery there are risks, but the alternative of not having your nerve damage addressed has far more downsides.
Dr. Seruya is a peripheral nerve surgery specialist. He is certified by the American Board of Plastic Surgery and has exceptional expertise and experience with nerve transfers and bypass grafting. His entire focus is peripheral nerve surgery.
So, while there are risks of further nerve damage, along with all of the risks inherent in any surgery, such as excessive bleeding, reaction to anesthesia, and the like, in these surgeries the rewards far outweigh the potential risks.
Schedule a Consultation
For additional information on Phrenic Nerve Paralysis and Paralyzed Diaphragm treatment in Los Angeles, CA, call our office at (310) 423-2129 to schedule a consultation today!